HEALTHCARE HUDDLE
Epic’s New AI Tools: How They’ll Impact Patients, Doctors, Systems
No matter how hard I tried, I couldn’t escape Epic this week. Nights on service had me glued to the chart. Mornings off had me scrolling LinkedIn to see everyone’s take on Epic’s newest AI features announced at its annual.
Oy vey—there’s a lot to catch up on. And the timing matters: Oracle announced its own AI‑backed EHR days earlier, raising the temperature on the AI/EHR arms race.
In this article, I’ll dive into some of the newest Epic features, highlight the GenAI wars, and then take a step back to view these features’ impact on patients, physicians, and the health system.
Epic’s Newest AI Features
At its annual User Group Meeting (which I was not invited to), Epic rolled out several new features—most of them powered by AI.
The headline announcement was three new AI scribes: one for patients, one for clinicians, and one for health systems.
Emmie (for patients): Think of Emmie as a digital assistant that helps patients get ready for their visits. It can schedule appointments, explain lab results in plain language, and even suggest when it’s time for health screenings.
Art (for clinicians): This is Epic’s partnership with Microsoft’s Dragon Ambient AI. Here’s how it works: you use Epic’s Haiku or Canto app to record the patient encounter, Dragon transcribes the conversation, and Epic turns it into a clinical note. Art can even tee up orders or prep a patient summary before the visit—like a digital resident that never sleeps.
Penny (for health systems): Penny is built for the back office. It combs through messy notes and unstructured data to improve coding, billing, and even denial appeals—essentially an AI scribe for the revenue cycle.
Epic also unveiled Cosmos, its predictive AI tool. Trained on 300 million patient records and 16 billion encounters across four countries, Cosmos is huge. One of its first uses is a tool that predicts a patient’s expected length of stay, which could help with discharge planning.
And finally, Epic announced Health Grid—a platform to better connect providers with payers, diagnostic labs, device makers, and telehealth companies. It feels like the kind of interoperability feature that should have existed years ago. On the patient side, Epic will launch MyChart Central, giving patients one login to access all of their Epic records, no matter which provider they see.
The Deets: GenAI Wars
We’re witnessing the GenAI war in healthcare—hundreds of startups chasing the same pool of practices and health systems.
First, we have the ambient AI folks who are transcribing physician-patient conversations into progress notes. Some go further, teeing up orders, suggesting billing codes, or even scheduling the next appointment. Here’s a market map from Elion—you’ll need to zoom in to appreciate just how crowded this space is.
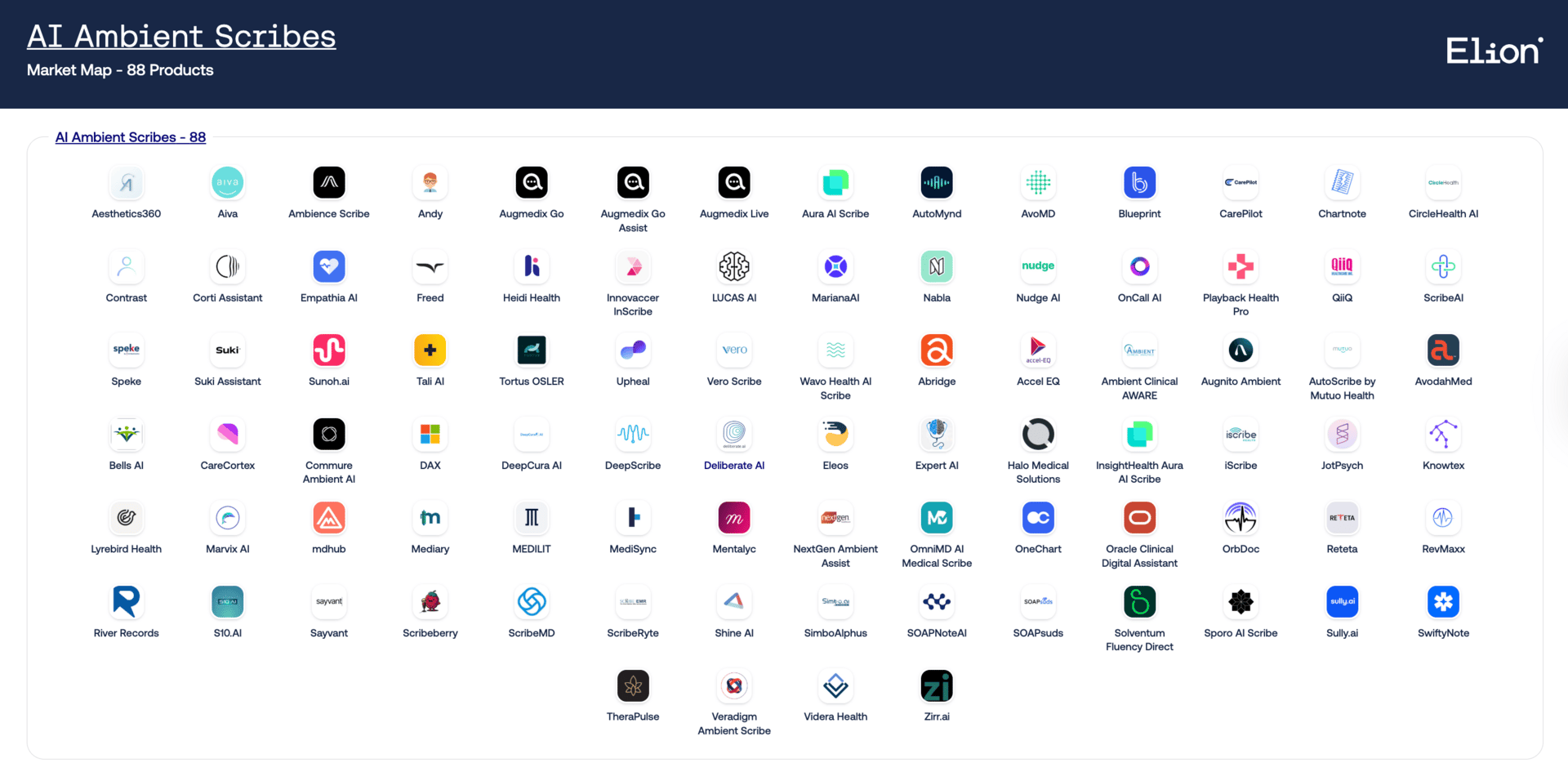
Source: Elion
Now Epic is rolling out tools that do all of that: transcription, pending orders, appointment scheduling. Interestingly enough, many of the startups on that very map already integrate with Epic.
Then there’s the summarization crowd—AI tools that sift through a patient’s chart and distill it down to what matters. I’ve been writing about this since 2022 when ChatGPT first hit the scene. Elion has another market map here.
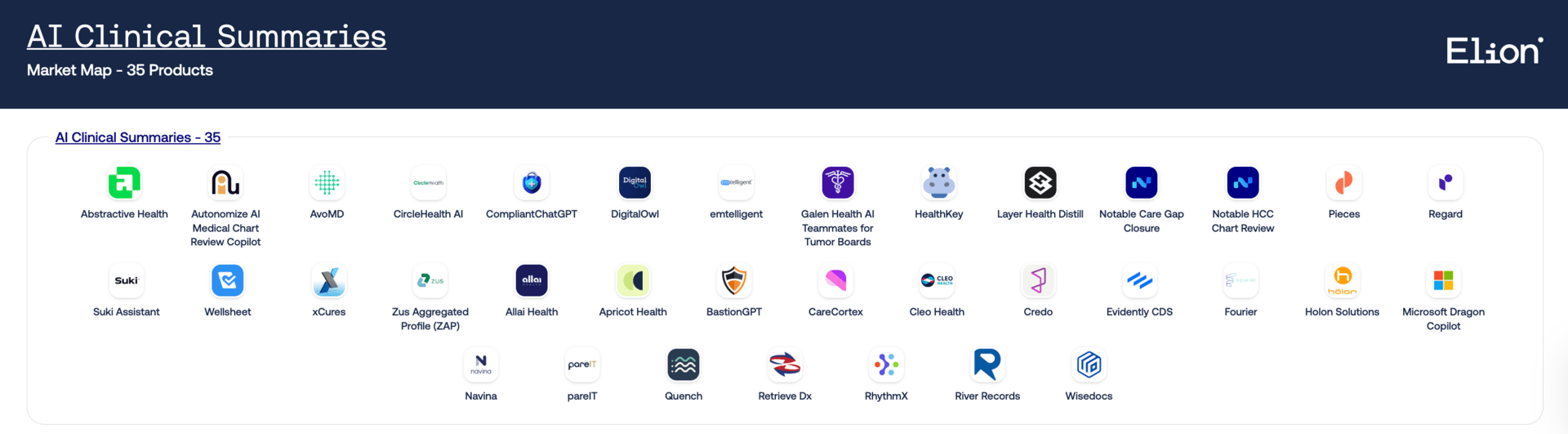
Source: Elion
And, once again, Epic is moving into that lane too. Its new features will summarize patient charts—and eventually let both patients and physicians chat with the chart.
It’s not just Epic. Oracle recently announced its own AI-powered EHR with similar capabilities.
Which raises the real question: if Epic and Oracle—by far the biggest EHR vendors—start offering these features natively, what happens to the startups? Is it game over?
Dashevsky’s Dissection
It took less than three years for Epic to build and now ship nearly everything I predicted back in my first ChatGPT article, The Future of Natural Language Processing in Healthcare, written in 2022. If you haven’t read it yet, I’d encourage you to check it out.
So, how will these new features actually impact patients, physicians, and health systems?
Patient
I see Emmie acting like an AI-patient advocate. Beyond scheduling and visit prep, its most valuable role could be helping patients truly understand their conditions. Take someone newly diagnosed with heart failure. In a rushed 15–30 minute visit, a physician explains the basics and prescribes medications. Afterward, Emmie could step in: explaining the disease in plain language, outlining the importance of GDMT medications, and even generating “must-ask” questions for the next visit. Instead of being left on their own after diagnosis, patients could finally have a guide walking them through the early, overwhelming steps of managing a chronic condition.
Physician
For doctors, it’s simple: any time not spent inside the chart is a win. Ambient documentation that auto-creates notes and pends orders will quickly shift from “nice to have” to the standard of care. And on the revenue side, Penny could tighten up documentation, reduce denials, and ensure accurate billing—helping physicians and practices capture revenue that too often slips away.
Health System
The big strategic question is what happens to startups when Epic and Oracle—the two EHR giants—start baking in the very tools those startups have been building. Jay Parkinson framed it well:
In my newsletter on Doximity’s acquisition of Pathway Medical, I laid out four keys to winning in the GenAI race:
Trust
Frictionless experience
Distribution moat
Specialty depth (optional, but powerful)
Epic and Oracle already check the first three boxes. They have physicians’ trust, they can deliver a relatively seamless experience with their new AI products, and they have unmatched distribution. Where they lag is specialty depth—tailored tools for cardiologists, pulmonologists, social workers, and beyond. That’s where startups still have room to differentiate. But to survive, they’ll need to nail trust, usability, and scale first.
In summary, Epic’s new AI features aim to empower patients, save physicians time, and help health systems capture more revenue—but they also tighten Epic’s grip as the central middleman in healthcare.
P.S. I created a repository of all my content covering AI in healthcare. Peruse at your leisure HERE.

THE MIDDLEMEN SERIES
Revenue Cycle Management: Why Healthcare’s Middleman Matters Most
Revenue Cycle Management might sound like dry admin work, but it’s the reason patients get surprise bills, doctors spend hours on paperwork, and hospitals live or die by razor-thin margins.
If you want to understand why U.S. healthcare feels so broken, you have to understand the middleman that moves the money.
👉 Read more details here.

INEFFICIENCY INSIGHTS
Why Dynamic Scheduling Could Be the Key to Cutting No-Shows
Long wait times and no-shows are the twin headaches of outpatient scheduling—and here’s the irony: the two are connected.
The longer a patient waits for an appointment, the more likely they are to cancel or never show up at all. Add in that no-show rates spike at certain times of day and in certain patient groups, and you start to see the real operational drain this creates.
We’ve thrown the usual fixes at the problem—patient portals, reminder texts, overbooking—but the data tells a different story about where the biggest opportunity might be. It’s not just about reminding patients to come… it’s about rethinking how we build the schedule in the first place.
👉 Full breakdown here.

HUDDLE #TRENDS
Medicare Advantage Explained: Growth, Profits, and Problems
Medicare Advantage was supposed to deliver better care at a lower cost.
Instead? It’s become a money-making machine for insurers—one that thrives on upcoding, prior auth denials, and favorable selection. Over half of all Medicare beneficiaries are now enrolled in MA plans, and yet the government is projected to overspend by tens of billions of dollars every year.
Even lawmakers—Republican ones—are calling it what it is: a “bastardized” version of the original vision.
So how did we get here? And what would it actually take to fix the system?
👉 See all my prediction updates here.

HUDDLE UNIVERSITY
Healthcare 101 Course
We were trained to take care of patients. But no one ever taught us how the system actually works:
How hospitals get paid.
Why your patient’s prior auth was denied.
What Medicare Advantage is doing to care delivery.
And why everything feels harder than it should.
That’s why I built this course: How Healthcare Really Works.
It’s short, visual, and built for people like us — physicians trying to make sense of the business and policy forces shaping our day-to-day work.
👉 Enroll in the course here.

NEW COURSE
Sponsor my next course: AI Meets Medicine
I’m launching a new course — AI Meets Medicine: 11 Practical Uses of Generative AI in Healthcare. It’s practical, evidence-based, and built for physicians and healthcare leaders.
I’m looking for one exclusive sponsor to make this course free for all 30,000+ Healthcare Huddle subscribers.
Reply to this email and I’ll send the details with the course syllabus.








