Patients are arriving at hospitals sicker than ever. Hospitals—especially urban ones—are chronically at capacity. Subacute rehab centers and skilled nursing facilities are capped. Emergency departments are consistently boarding patients. Hospital margins remain razor thin.
What can we do about this?
If we tackled this problem as I do in my Inefficiency Insights reports, we'd find countless root causes. But today, I want to focus on one: hospital capacity. One promising solution is Hospital at Home programs.
In this #Trends report, I'll dive into the capacity problem, explain Hospital at Home, review current policy and market trends, and close with a prediction about acute care's relationship with the inpatient setting.
The Problem: Inpatient Bed Capacity
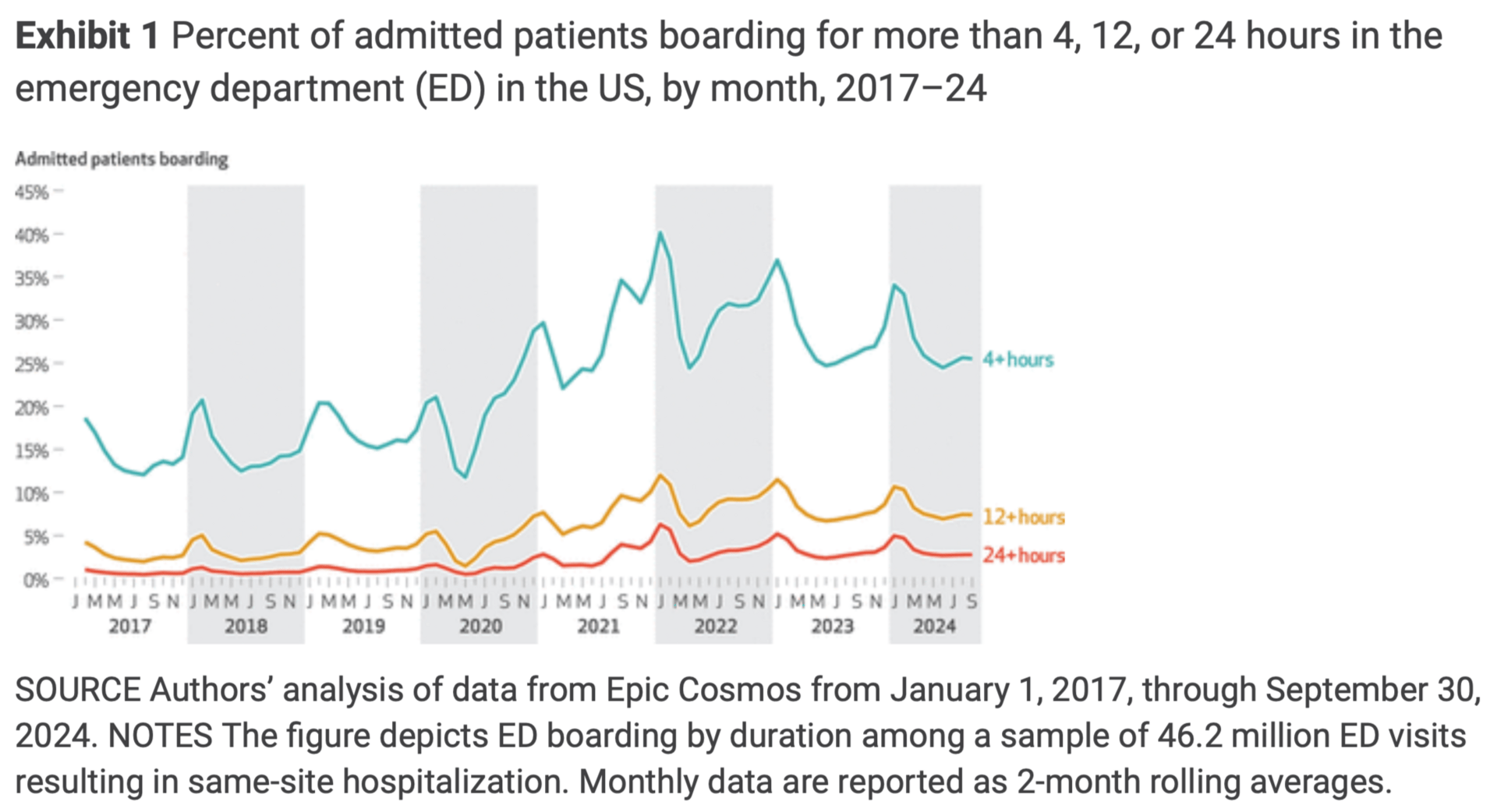
The main symptom of hospital capacity strain—when available inpatient beds are scarce—is emergency department boarding. Admitted patients end up waiting in the ED for a bed upstairs to open. The irony? A bed upstairs only becomes available when a bed at a subacute rehab (SAR) or skilled nursing facility (SNF) opens up for discharge. That's the bottleneck.
Boarding is dangerous, and the problem has only worsened since the pandemic. Waiting 4+ hours for a bed in the ED is now common—almost expected. You can imagine the risks this poses to older adults: delirium, falls, and more.
Patient care suffers, but so does the hospital's bottom line. A patient upstairs who's medically ready for discharge sits waiting for a SAR bed. Meanwhile, they're occupying an inpatient bed that could be used for the patient boarding in the ED—or for a higher-paying elective procedure.
This is where hospital at home comes in.
The Solution: Hospital at Home
Hospital at Home (HaH) is a care delivery model allowing patients who require an acute-level of care to receive it in the comfort of their homes instead of the inpatient setting. The model was birthed to address several challenges that chronically impact hospitals:
Hospital capacity constraints (see above)
Rising healthcare costs
Need for patient-centered care
Hospital at Home 101
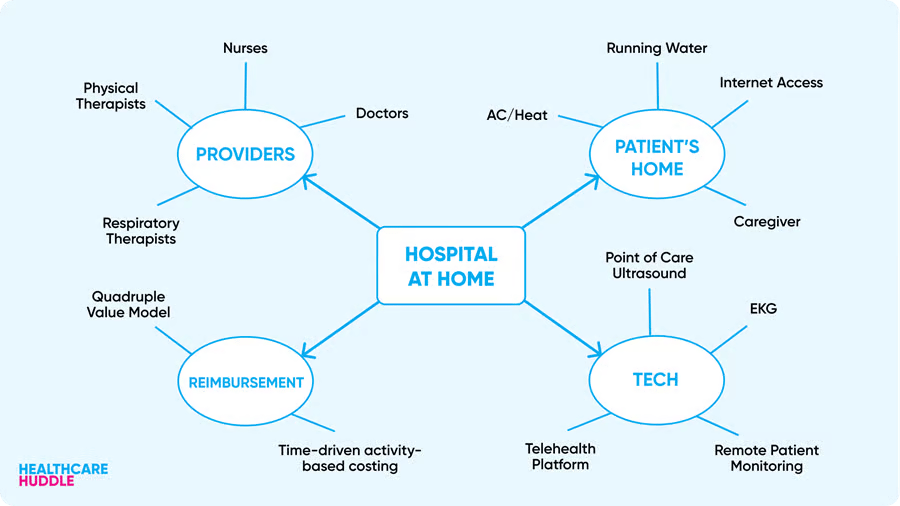
The HaH model leverages a multidisciplinary team—including physicians, nurses, pharmacists, and allied health professionals—supported by telehealth, remote patient monitoring, and robust logistics to deliver acute care for common, treatable conditions like respiratory, circulatory, renal, and infectious diseases.
Services range from medication administration and vital sign monitoring to diagnostic testing and coordinated care planning.
Key characteristics include:
Acute Care at Home: Targeting patients who would otherwise be hospitalized.
Hybrid Care Delivery: Blending in-person visits with telehealth and remote monitoring.
Patient Selection: Rigorous criteria ensure only clinically appropriate, stable patients with suitable home environments are enrolled.
HaH is not new. Its roots trace back to the UK in the late 1970s, with subsequent adoption in countries with centralized health systems such as Italy, Australia, Canada, and Israel. The U.S. first experimented with HaH in the late 1990s, notably through Dr. Bruce Leff’s pioneering work at Johns Hopkins, focusing on older adults to reduce risks from prolonged hospital stays.
Despite promising early results, HaH adoption in the U.S. was slow due to lack of robust reimbursement models, limited physician buy-in, and insufficient technology for remote monitoring and care coordination.
The COVID-19 pandemic was an evident turning point for HaH.
Upgrade to Huddle+ to continue reading.