HEALTHCARE HUDDLE
Mental Health Meets Tech: What Care Looks Like in 2035
Wearable devices have completely changed how we think about personal health. What started with tracking steps and resting heart rate has evolved into real-time insights about our bodies—and now, even our minds.
Mental health is no longer being left behind.
Over the years, I’ve written about how mental healthcare might evolve as technology improves. (If you’re curious, check out Tech Meets Mind: Wearable Technology in Mental Health Care and Mental Health Care in 2032.)
Now feels like a good time to revisit those ideas—update a few things, reflect on what’s changed, and look ahead to what mental healthcare could look like in 2035.
The Deets: Wearable Technology and Mental Health
Wearable tech can track three big buckets of data:
Fitness activity: steps, pace, cadence, GPS, elevation, etc.
Physiology: resting heart rate (RHR), heart rate variability (HRV), blood pressure, oxygen levels, respiratory rate, sleep, blood sugar, even single-lead EKGs.
Behavior: fall detection, sedentary time, gait, even close-contact alerts (think: Covid-19).
You’ll find these sensors in all sorts of things—watches, rings, clothing, skin patches, you name it.
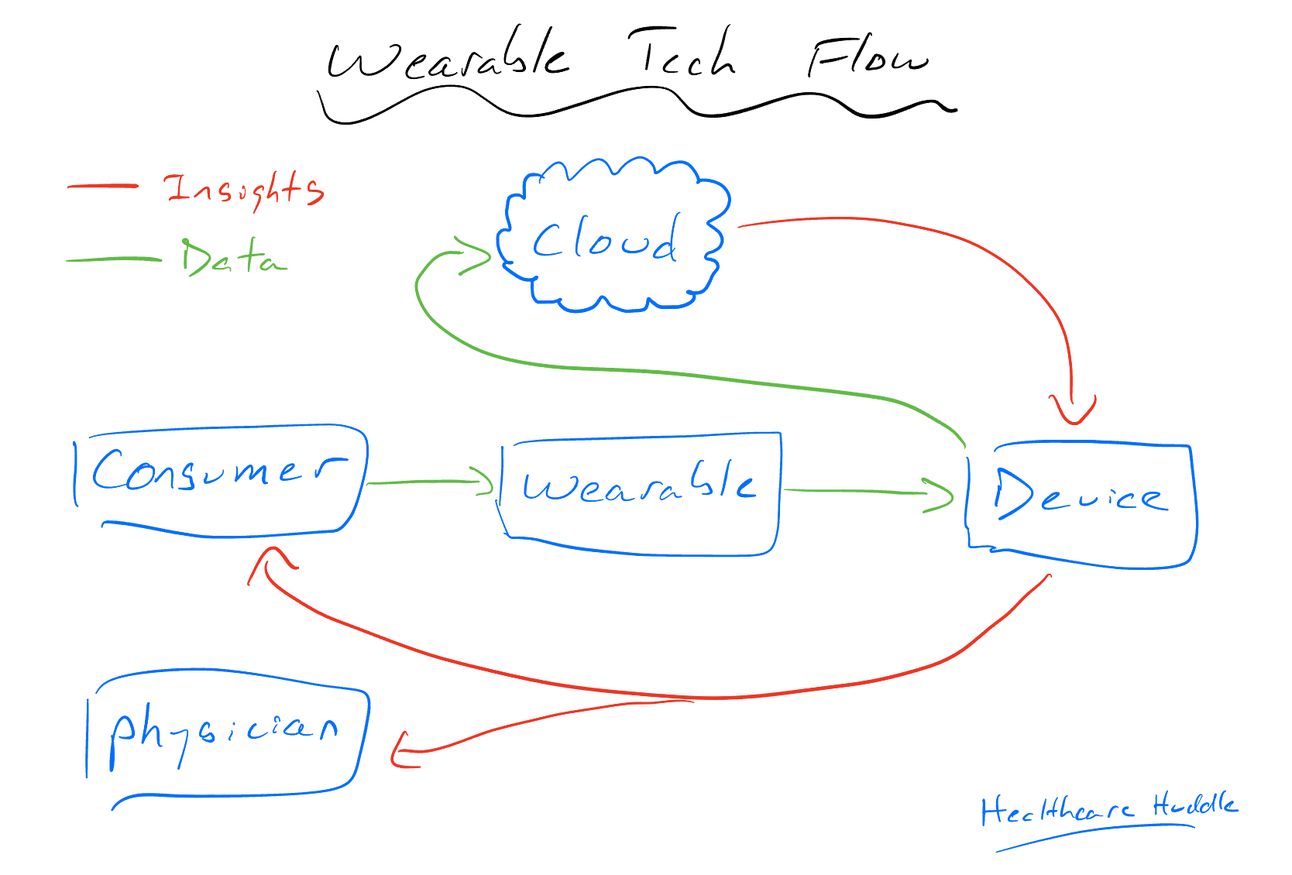
No matter the form, the process is the same: the wearable collects data, sends it to your phone, gets processed in the cloud, spits out insights for you or your doctor.
When it comes to mental health, wearables can offer real-time context that complements what happens in a clinic. Take depression, for example.
Depression affects sleep, energy, activity, and appetite—all things a wearable can help track. Sleep and movement are directly measured. Energy can be inferred from your heart rate, step count, and how much time you spend lying around. Even appetite might be estimated if the wearable tracks weight and food intake.
Worn consistently over time, these devices can paint a picture of mental health that’s hard to get from a 15-minute office visit.
Mental Health Wearable Tech Space
Here’s a quick look at how different wearables are tackling mental health.

Fitbit: Devices like the Sense 2 and Charge 6 track mood, HRV, skin temp, and electrodermal activity for stress insights.
Oura: Oura’s Daytime Stress feature uses HRV, heart rate, temperature, and breathing to classify your stress state in real time—Stressed, Engaged, Relaxed, or Restored. It gives users a daily picture of how their body responds to life’s ups and downs, turning wearables into powerful mental wellness tools.
Feel Therapeutics: Uses continuous biometric, behavioral, and clinical data to power digital mental health programs.
Apollo Neuro: Delivers soothing vibrations to the skin to help retrain the nervous system and reduce stress.
Apple Watch: Offers emotion tracking and mood assessments, with built-in tools to help users reflect and identify mental health patterns.
Lief Therapeutics: Tracks HRV in real time and provides biofeedback via gentle vibrations, plus personalized coaching.
Muse: EEG-powered meditation headband offering real-time feedback on brain activity, heart rate, and breath.
WHOOP (my favorite): Combines sleep and recovery data with daily journaling to surface how life stressors affect your health.
Garmin: Supporting research that links wearable data with mental health outcomes—something I’ve been excited about since my early Garmin days as a teen runner.
Dashevsky’s Dissection
By 2035, I’d bet that 9 out of 10 patients will be wearing something that monitors their health—whether it’s a ring, wristband, patch, shirt, or even a smart earring.
These wearables won’t just track steps and sleep. They’ll be deeply integrated with large language models (LLMs), which by then will be far more advanced than what we’re using today. Think of the LLM as a kind of middleman—or more accurately, a real-time agent. It’ll continuously interpret wearable data, flag early signs of mental health decline, and even ping your physician if intervention (or prevention) is needed.
As tech becomes more embedded in our daily lives, mental health concerns will only become more prevalent. But wearables could help us stay grounded—offering a feedback loop between mind, body, and care team.
From the patient’s perspective, this looks like personalized, always-on mental health support. You’re logging feelings and seeing how your body is responding in real time and getting nudges when something’s off.
From the physician’s perspective, more data is a good thing—if it’s usable. Imagine combining ambient AI that listens in on therapy sessions (yes, I know this is controversial) with wearable data. That fusion could uncover deeper trends—like changes in HRV or sleep patterns that correlate with stress levels or treatment response. If someone starts Lexapro, and suddenly their wearable shows better sleep and lower stress markers, that might serve as an early signal the medication is working.
At the system level, the big question is: how do we pay for this?
Right now, there’s no clear reimbursement model for clinicians who use LLMs or wearable data in care. And if these devices are going to guide medical decisions, shouldn’t they be FDA-approved? That approval process isn’t built for the pace of tech innovation—but I’d expect we’ll see a new regulatory and reimbursement framework by 2035 to support this shift.
Once that happens, I think we’ll see widespread use of wearable tech—not just for fitness or fun—but as a core tool in managing mental health.
In summary, wearable technology is quietly reshaping mental health care. From tracking sleep and stress to offering real-time feedback, these devices are becoming powerful companions in both self-monitoring and clinical care. As large language models evolve and integrate more deeply with wearables, we may soon see a future where early detection, treatment monitoring, and even preventive care are automated, personalized, and always-on. The only thing standing in the way? Reimbursement and regulation. But by 2035, that might finally catch up.

🔒 PREMIUM CONTENT THIS WEEK
What you’re missing
While you’re reading this, Huddle+ members are diving deeper into the topics that matter most.
Here’s what they saw this week:
The Middlemen Driving Up Drug Costs: A breakdown of how pharmacy benefit managers (PBMs) work, why they exist, how they make money—and why they’re under fire. If you think you understand the drug supply chain, think again.
Should Insurance Pay for Primary Care? I break it down through three lenses—an economist, an engineer, and a physician—to unpack why our payment model might be hurting care more than helping it.
How Healthcare Really Works: The system is more than just medicine. This new Huddle University course explores the hidden forces shaping healthcare: hospital finances, insurance games, drug pricing, and more.
If you’re serious about understanding the business behind the practice—and want to grow your impact—upgrade here.

COMMUNITY POLL
Fill out these questions below!!!!!
Fill out this form if you’re interested in small, niche in person meet ups (Huddle+ members would get priority).
Let me know, too 👇
