Of all the inefficiencies in healthcare, prior authorization is the most fascinating bottleneck to me. Not because of the inefficiency itself, but because of the solutions surrounding it.
Last week, I reported on AI-powered patient engagement and why it's the area in healthcare with the most potential for AI growth. The piece was inspired by a Menlo Ventures report on the state of AI in healthcare. The report also mentioned that prior authorization AI spending is growing 10x year-over-year—from $10 million in 2024 to $100 million in 2025.
The timing feels right to dig deeper.
In this article, I'll cover the background on prior authorization, who's solving the problem, and the broader impact of these solutions on patients, physicians, and health systems.
The Deets: Prior Authorization
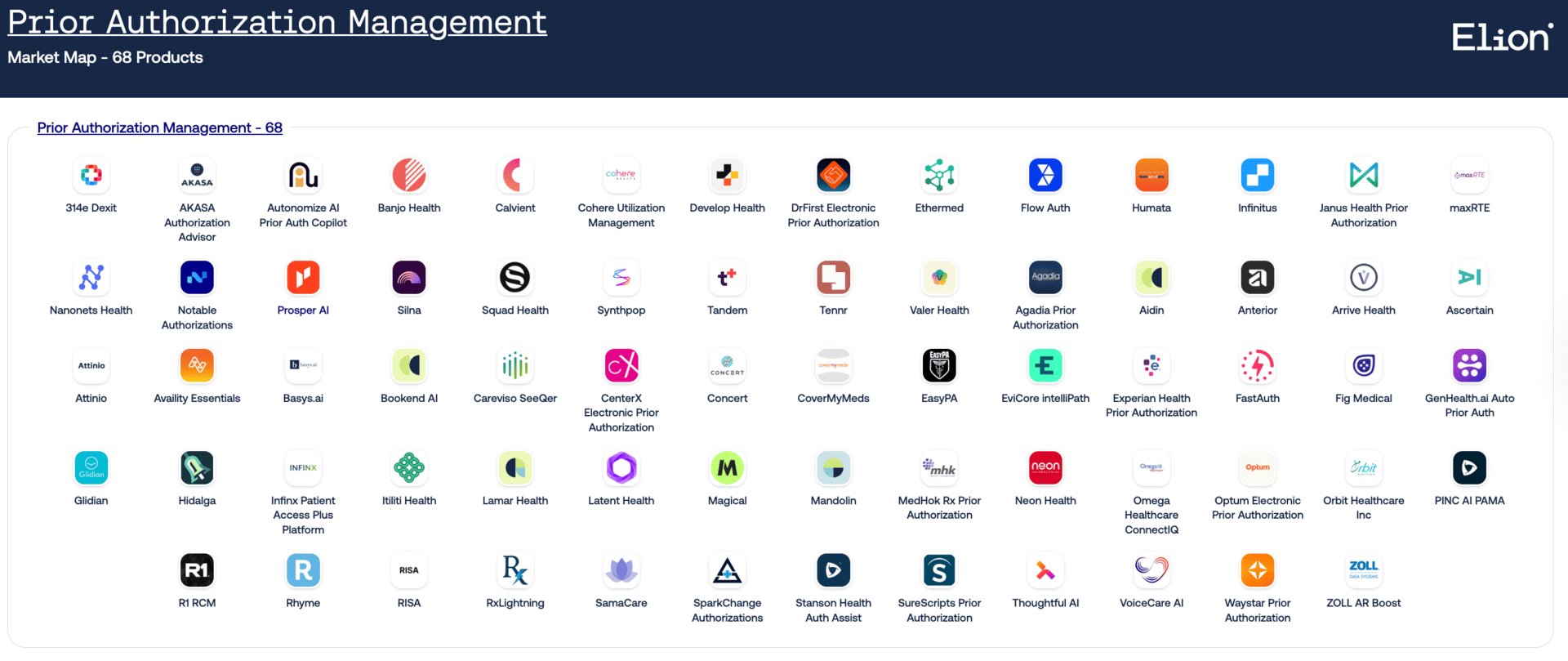
I first wrote about prior authorization in 2022, highlighting how Medicare Advantage plans were using AI to deny claims left and right. Yes, insurers have been deploying AI for years—and now, slowly, the physician and provider side is catching up. I've included a graphic below that demonstrates the prior authorization process at a high level. The bottlenecks are easy to spot.
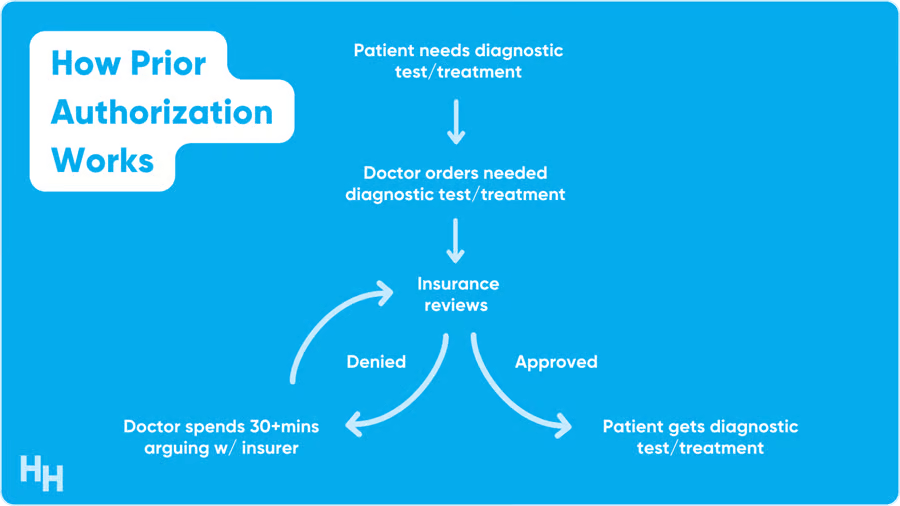
Here's what this looks like in practice.
You're treating a patient with moderate-to-severe rheumatoid arthritis who has failed methotrexate and sulfasalazine.
You want to start a biologic—adalimumab seems like the obvious next step.
But before your patient can get the medication, you need prior authorization.
Your nurse spends 45 minutes on hold with the insurer, pulling clinical notes from the EHR, filling out forms, and explaining why step therapy is complete.
Three days later, the prior auth gets denied.
The insurer wants to see one more failed DMARD first.
Your patient waits another eight weeks while you trial hydroxychloroquine, knowing it probably won't work. Meanwhile, their joints are getting worse.
A mess!
Who’s “Solving” the Prior Auth Problem?
As stated in the Menlo report, prior authorization is becoming a popular space to invest AI on both sides of the table: insurers and physicians. The former group has been in the AI game for a while, but now physicians are gaining some power with AI to fight denials.
Some data below:
AI prior authorization spending is growing 10x year-over-year from $10 million in 2024 to $100 million in 2025.
Significant services-to-software conversion opportunity ($98B admin spend, only 3% software)—huge market.
Some startups have already recognized this problem and are helping physicians out with prior authorization by using AI:
Latent Health: clinical AI to automate prior authorizations, benefits checks, and appeals for specialty pharmacies by pulling data directly from the EHR.
Tandem: AI platform that plugs into the EHR to handle the entire medication access workflow—from benefits checks to PA submissions, appeals, copay assistance enrollment, and pharmacy routing.
Mandolin: AI platform that automates buy-and-bill workflows for infusion centers, including payer policy management, financial assistance, and prior authorizations—all directly within the EHR.
Squad Health: automates prescription admin work—prior auths, appeals, copay help, and pharmacy routing—using AI.
Silna: automates prior authorizations, benefits checks, and eligibility tracking for specialty providers in physical therapy, speech therapy, and behavioral health.
Tennr: automates prior authorizations, patient intake, and eligibility checks by using AI to pull data directly from faxes and other medical documents.
Flow Auth: an AI tool that handles the full prior authorization process—from detection to submission to appeals—by syncing with EHRs and payer portals to auto-fill documentation based on each payer's medical necessity rules.
Notice the pattern? These tools all focus on pulling data from the EHR and auto-filling payer forms. They’re making the existing process faster, not questioning whether the process should exist at all. Some specialize in specialty pharmacy and infusions, others in outpatient care or specific provider types, but the core value proposition is the same: automate the paperwork, reduce the time burden, and get claims through faster. That's textbook efficiency AI. This highlights the broader challenge we're facing in healthcare technology.
Efficiency AI vs. Transformative AI
I've written before about the difference between efficiency AI and transformative AI. Efficiency AI automates existing workflows and makes broken processes faster. Transformative AI redesigns or eliminates those processes entirely by addressing root causes.
Prior authorization AI is almost entirely efficiency AI. We're not asking whether prior authorization should exist in the first place, we're just making it less painful. Both physicians and payers are investing in AI to speed up the same adversarial process, each side trying to gain an advantage. Physicians get faster approvals and fewer denials. Payers get faster triage and better detection of low-value claims. But the fundamental problem—misaligned incentives and fee-for-service payment models—remains untouched.
Interestingly, some payers are already recognizing the threat. UnitedHealth just launched Optum Real, a "real-time claims system that delivers instant coverage validation and improved claims accuracy." Physicians now know instantly at the point of care what's covered. Patients are more aware of their coverage status before leaving the appointment. It's a smart move. UnitedHealth is getting ahead of the provider-side AI wave by making their own approval process faster and more transparent. But again, this doesn't address the root cause of the problem. It just speeds up the dysfunction.
Dashevsky's Dissection
I don't see either physicians or insurers "winning" the AI race in prior authorization. I just see one of them "losing" less. For physicians, this means less time dealing with the clunky prior authorization process. For insurers, this means fewer losses when triaging unnecessary claims. None of the AI solutions truly address the root cause.
We essentially have an escalating AI arms race. This reminds me of Doximity's mobile fax feature, which I love—but it truly just helps streamline the dysfunction of needing to fax in the first place!
So how do these AI solutions—designed to streamline prior authorization on both sides—impact stakeholders?
For patients, they're caught in the middle of the brawl. With AI, the brawl will be shorter, perhaps as quick as ripping off a bandaid. Faster approvals mean less treatment delay, which is undeniably better. But patients are still subject to the same underlying gatekeeping, just with quicker turnaround times.
For physicians, these solutions remove the prior authorization burden. Either we'll be alerted at the point of care that PA is needed, avoiding delays in care, or the denial process is streamlined, only involving us if absolutely necessary. That's a win for our time and sanity. But it doesn't solve the deeper issue: clinical decisions are still being second-guessed by algorithms trained on cost containment.
For payers and health systems, the stakes are higher. Now that physicians are building their own AI weapons to fight claims denials, insurers face two dominant fears:
Surging call and claims volume. AI-enabled prior authorization tools let providers submit claims instantly, check status, and file appeals at scale. Payers must staff against this flood or risk being overwhelmed.
Risk of increased costs. Coding tools trained on vast data sets are designed to identify missed revenue opportunities and optimize billing codes to maximize reimbursement. Payers fear approving and paying for unjustified procedures while also feeling pressure to improve turnaround times.
Payers are responding by updating policies around medical necessity, increasing audits, and working with AI platforms like Distyl to stand up their own AI systems to match provider capabilities. It's an arms race with both sides investing in AI to fight the same battle more efficiently, neither addressing why the battle exists in the first place.
In summary, prior authorization AI is a perfect case study in healthcare's tendency to automate dysfunction rather than fix it. These tools will save physicians time and reduce administrative burden, and that's genuinely valuable. But we should be clear about what we're getting: a faster version of a broken system, not a better one.

SPONSORED BY HUDDLE UNIVERSITY
New course on how AI can improve healthcare utilization, launching November 9th. Here's what you'll learn:
How hospitals are using AI to optimize clinical operations and improve quality
How physician groups are reducing no-shows and managing value-based care populations
How payers are streamlining prior authorization and detecting fraud
The adoption challenges (and how to overcome them)
Pre-enrollment is open at $149 (regular price: $199).

THE MIDDLEMEN SERIES
Pharmaceutical Wholesalers: The Middlemen Who Control 92% of U.S. Drug Distribution
Healthcare wholesalers move 92% of prescription drugs from manufacturers to your hospital pharmacy. They're the invisible logistics layer that keeps medicines flowing—but their market concentration and thin margins make the entire supply chain vulnerable to shortages and disruptions.
👉 Read more details here.

HUDDLE #TRENDS
The Direct-to-Consumer Lab Testing Boom: Should You Care?
WHOOP just launched blood testing. OURA offers 50+ biomarkers for $99. Function Health raised $400 million to test 160 biomarkers annually. The direct-to-consumer lab testing market hit $3.6 billion in 2024 and shows no signs of slowing down.
But here's the question I keep asking: if comprehensive biomarker tracking truly improved clinical outcomes, wouldn't we already be doing it in standard practice? Most routine checkups are well-covered by a CBC, BMP, lipid panel, and A1c. So when your otherwise healthy patient shows up with a longevity panel revealing a mildly elevated inflammatory marker, what do you do?
The answer depends on understanding who this market really serves—and the data reveals something uncomfortable about where we're heading...
👉 Full breakdown in my latest Huddle #Trends report here.

INEFFICIENCY INSIGHTS
Apple Watch Asthma Study Shows Wearables Work—But Not for Everyone
60% of adults with asthma have uncontrolled disease. Not because treatments don't work—they do. But because we've designed asthma management around 15-minute clinic visits instead of the environments where patients actually live.
A JAMA trial from Apple and Elevance tested whether wearables could change this. 901 adults. Apple Watch plus AI-driven nudges. 12 months of follow-up. The results showed a 2.8-point improvement in asthma control scores—approaching clinical significance. Promising for a scalable intervention.
Interestingly enough, for African American participants, the benefit disappeared completely. Engagement dropped by 2.4x. And the populations bearing the heaviest asthma burden are the same ones our digital tools are failing to reach.
This is a design problem, not a technical one. And the fix is more obvious—and more actionable—than you might think…
👉 Full breakdown in my latest Inefficiency Insights article here.