HEALTHCARE HUDDLE
AI-Powered Patient Engagement: The $100B Healthcare Gap
Menlo Ventures released its State of AI in Healthcare Report, which I found informative during my 5 AM Friday morning writing session—racing to finish the Huddle before my daughter wakes up. The report focused heavily on AI scribes, which are old news in my opinion. Scribes are becoming the "pager" of healthcare: everyone has one, and if you don't, something's wrong.
But there's an area with immense potential I want to focus on—patient engagement. Reviewing my prior Inefficiency Insights reports, I realized I discuss patient engagement frequently but rarely label it explicitly. I've covered everything from why HCAHPS surveys fail to digital nudges in primary care, AI-powered discharge summaries to Epic's SMS scheduling feature. I'm basically giving away million-dollar startup ideas in every article! (Half joking.)
Today, I'll highlight the issues plaguing patient engagement and why it deserves attention, explore the AI-driven patient engagement market, and offer my take on the impact for patients, physicians, and health systems.
Challenges: Patient Engagement
Patient engagement fails after clinical care ends. I see this frequently in my discharge work. Through my Timely Transitions QI initiative, I've mapped every breakdown in communication, handoffs, and discharge planning. For example, we discharge patients with jargon-filled summaries written for their PCPs—not for them. They leave confused about medications and follow-up instructions, and with no one checking whether they understand.
But problems start earlier—even before the hospital. Patients wait weeks for appointments while others cancel or no-show—a mismatch that inspired me to build Nayroo, a dynamic scheduling platform. How can I book a Genius Bar appointment to fix my iPhone in 30 seconds, but patients wait 20 minutes on hold to book a doctor's visit?
After appointments or hospital stays, patients enter a dead zone. We abandon them between touchpoints.
COPD readmissions are failures of communication, access, and coordination—not clinical failures.
Patients get called with results they don't understand.
Patients are told they have "community-acquired pneumonia" without explanation.
Patients receive discharge instructions, but no one follows up to see if they filled prescriptions, understood the plan, or know when to return.
The engagement challenge is closing gaps where patients fall through: between hospital and home, specialist and primary care, diagnosis and understanding. These are human communication problems at scale—not just technology problems, which is where AI-powered patient engagement tools can make a difference.
AI-Powered Patient Engagement: The Market Opportunity
Per the report, patient engagement and access account for more than $100 billion in annual administrative spending, yet software captures only about 5% of that total. 5%! So much room for disruption, which is exactly what AI is doing. AI is creating a $100+ million market that grew 20x year over year.
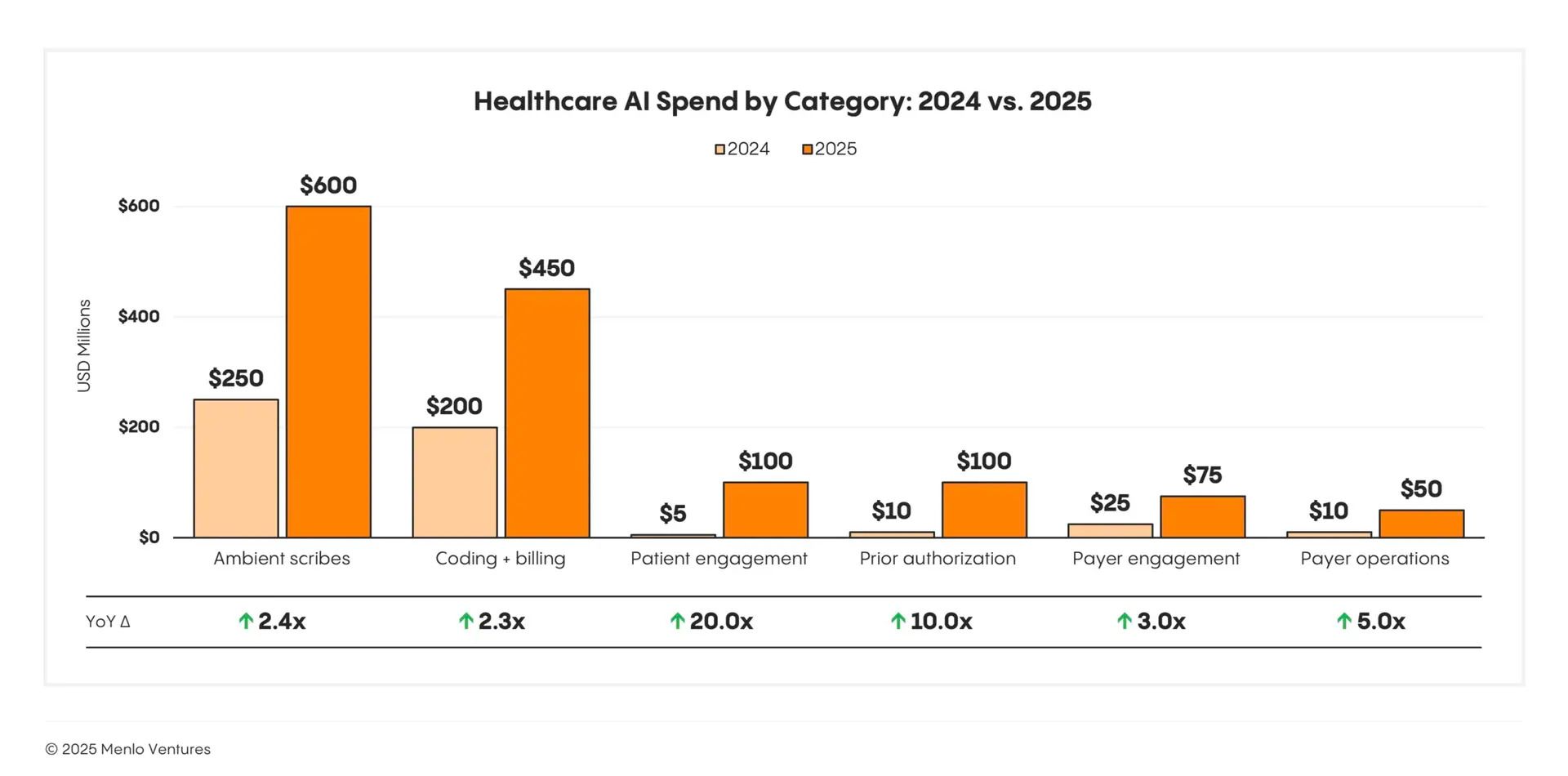
Source: Menlo
The main reason for this market growth is simple: AI can finally operate at the scale needed to close those communication gaps I just described above.
The Menlo report breaks the market into four main categories, and each addresses a specific failure point in patient engagement:
Consumer wellness platforms like Function Health, Ash, and SuppCo help people take control of their own health through biomarker monitoring, lifestyle tracking, and always-available engagement. These tools shift engagement upstream—before patients even enter the healthcare system. I have my thoughts, though, about the lab testing space—read them here.
AI triage platforms like Doctronic, Counsel Health (founded by Sinai doc!), Torch Health, and Roon assess symptoms conversationally and route patients to the appropriate level of care. They solve the front-door problem: helping patients figure out where to go and when.
Scheduling automation solutions like Assort Health, Hello Patient, and Clarion eliminate manual appointment booking and patient triage. This is the space I was trying to crack—trying to match patients to open slots automatically and reduce no-shows (pre-AI).
Care navigation platforms like Hippocratic AI, Ellipsis Health, Kouper Health, Ferry Health, and Solace Health manage ongoing patient communication. They call with results. They schedule follow-ups. They answer questions. They coordinate care transitions. These platforms address the dead zone I described—the abandonment that happens after clinical encounters end.
This last category is where the biggest opportunity lies. Providers historically don't follow up with patients because the responsibility falls to overburdened nurses or outsourced call centers. AI agents can finally make post-discharge engagement scalable and consistent (see Aidify here).
The market is moving fast because the ROI is immediate. Or so I hope. Better engagement means fewer readmissions, better medication adherence, higher patient satisfaction scores, and improved outcomes. Health systems are starting to see these tools not as nice-to-haves but as essential infrastructure for modern care delivery.
Dashevsky's Dissection
These patient engagement AI tools promise to be transformative AI—addressing the root cause of engagement failures—rather than efficiency AI that automates a broken process. But the question is whether they actually deliver on that promise.
Impact on Patients
The potential benefits are clear. Patients gain more ownership of their care plans, leading to better medication adherence and fewer missed appointments. They arrive prepared with questions, rather than leaving confused. They get follow-up calls that check understanding and coordinate next steps. This should reduce unnecessary readmissions and ER visits.
However, not every patient has a smartphone or digital literacy. Language barriers and cultural nuances matter—can AI handle a Spanish-speaking patient with limited health literacy explaining acute sinusitis? Probably. But trust is another issue. Will patients trust an AI calling with test results, or will they demand to speak to a nurse anyway? And there's a real risk that these tools will widen disparities: engaged patients with resources get better follow-up, while vulnerable populations fall further behind.
Impact on Physicians
These tools should lift a heavy burden: ensuring patients understand every aspect of their care plan—medications, diagnostics, insurance, social work. Much of that communication falls outside our scope of practice but still ends up on our plate. AI can fill those gaps at scale.
But does it actually reduce our workload? Maybe not. We might end up reviewing AI-generated communications before they go out. More informed patients mean more questions—which is good for care, but could eat up time we don't have. And when AI gets something wrong or a patient needs escalation, that falls back on us. The liability question is real: if an AI agent gives incorrect discharge instructions and the patient gets readmitted, who's responsible? Right now, it’s us physicians.
Impact on Health Systems
At scale, the value proposition is compelling. Lower 30-day readmissions save money. Reduced malpractice risk from better-informed patients saves money. Better appointment adherence for specialties and diagnostics generates revenue. Streamlined referrals keep patients in-network.
But the ROI is still mostly projected, not proven. Implementation costs shouldn’t be ignored—integration with EHRs, training staff, managing vendor relationships. And if these tools create more physician work instead of less, health systems face burned-out clinicians on top of the technology spend.
Whether AI will actually close the gaps or just create more efficient abandonment is the question.
We need to see:
Proven outcomes data, not just engagement metrics
Transparent AI decision-making that physicians can review and override
Integration that doesn't add physician work
Equity safeguards built into deployment strategies
These tools have real potential. But transformative AI requires transforming the system, not just automating it. The jury's still out on whether patient engagement AI will deliver on that promise.

SPONSORED BY HUDDLE+
New course on how AI can improve healthcare utilization, launching November 9th. Here's what you'll learn:
How hospitals are using AI to optimize clinical operations and improve quality
How physician groups are reducing no-shows and managing value-based care populations
How payers are streamlining prior authorization and detecting fraud
The adoption challenges (and how to overcome them)
Pre-enrollment is open at $149 (regular price: $199).

THE MIDDLEMEN SERIES
Pharmaceutical Wholesalers: The Middlemen Who Control 92% of U.S. Drug Distribution
Healthcare wholesalers move 92% of prescription drugs from manufacturers to your hospital pharmacy. They're the invisible logistics layer that keeps medicines flowing—but their market concentration and thin margins make the entire supply chain vulnerable to shortages and disruptions.
👉 Read more details here.

HUDDLE #TRENDS
The Direct-to-Consumer Lab Testing Boom: Should You Care?
WHOOP just launched blood testing. OURA offers 50+ biomarkers for $99. Function Health raised $400 million to test 160 biomarkers annually. The direct-to-consumer lab testing market hit $3.6 billion in 2024 and shows no signs of slowing down.
But here's the question I keep asking: if comprehensive biomarker tracking truly improved clinical outcomes, wouldn't we already be doing it in standard practice? Most routine checkups are well-covered by a CBC, BMP, lipid panel, and A1c. So when your otherwise healthy patient shows up with a longevity panel revealing a mildly elevated inflammatory marker, what do you do?
The answer depends on understanding who this market really serves—and the data reveals something uncomfortable about where we're heading...
👉 Full breakdown in my latest Huddle #Trends report here.

INEFFICIENCY INSIGHTS
When Patients Can't Afford Life-Saving Medications
The U.S. healthcare system has much to love and hate—but what I hate most is when patients can't access the care and medications they need. As a physician, I feel truly hopeless when a patient needs a medication or follow-up appointment but can't afford it or access it because of their insurance status. It's terrible.
Recently, I cared for a patient who made me feel exactly this way: uninsured, no access to care. His hospitalization was the first time he'd interacted with the healthcare system in decades. He came in with worsening shortness of breath. We found a massive clot in his lungs, plus uncontrolled type 2 diabetes, plus high blood pressure, plus high cholesterol. In the hospital, treatment was straightforward: apixaban for the lung clot, insulin for diabetes, olmesartan for blood pressure, and a statin for cholesterol.
But discharge planning became a nightmare…
👉 Full breakdown in my latest Inefficiency Insights article here.