HEALTHCARE HUDDLE
Traditional Medicare's New AI Prior Auth Problem
Traditional Medicare will test prior authorization artificial intelligence in select states starting January 2026 under the WISeR (Wasteful and Inappropriate Service Reduction) Model—a new CMS initiative to reduce unnecessary services, fraud, waste, and abuse.
Seems appropriate, right? The government showing some tech savvy to improve healthcare costs.
But this is prior authorization we're talking about! The thing physicians and patients dread most about our healthcare system!
In this article, I'll highlight prior authorization in Traditional Medicare, dive into the WISeR model, and discuss the potential impacts on patients, physicians, and Medicare.
Prior Authorization in Traditional Medicare
Currently, the prior authorization process under Traditional Medicare works well (I want to emphasize: this is Traditional Medicare, not Medicare Advantage—where prior authorization is not great). Only around 50 outpatient medical services require prior authorization under Traditional Medicare, and the process is straightforward.
Medicare Administrative Contractors review each prior authorization quickly.
These contractors' prior authorization decisions are nearly 100% accurate.
The Traditional Medicare prior authorization process is highly accurate and prevents waste—without delaying or denying necessary care.
Prior Authorization Under Medicare Advantage
Prior authorization under Medicare Advantage is a different story. It faces intense criticism, especially regarding AI-driven claims reviews. Unlike Traditional Medicare, MA plans require prior authorization for countless services. In 2023 alone, MA plans made nearly 50 million prior authorization determinations—up from 37 million in 2021. For comparison, Traditional Medicare reviewed 400,000 prior authorizations total in 2023. Around 11% of MA's denied claims were appealed, and of those appeals, roughly 80% were overturned—raising the question: should they have been denied in the first place?
As a Reminder: Physicians Hate Prior Authorization
Physicians truly despise prior authorization. It limits autonomy, delays care, and consumes valuable time.
Delayed care: 93% of physicians surveyed say prior authorization results in delayed care.
Serious adverse events: 29% of physicians say prior authorization led to a serious adverse event for a patient in their care.
Burnout: 89% report that prior authorization somewhat or significantly increases physician burnout.
The Details: The WISeR Model
CMS launched the WISeR Model to reduce unnecessary clinical care, fraud, and abuse by contracting with AI companies experienced in prior authorization to expedite and improve the claims review process. The idea is that AI-assisted claim reviews will eventually decrease costs and reduce the administrative burden on physicians navigating prior authorization.
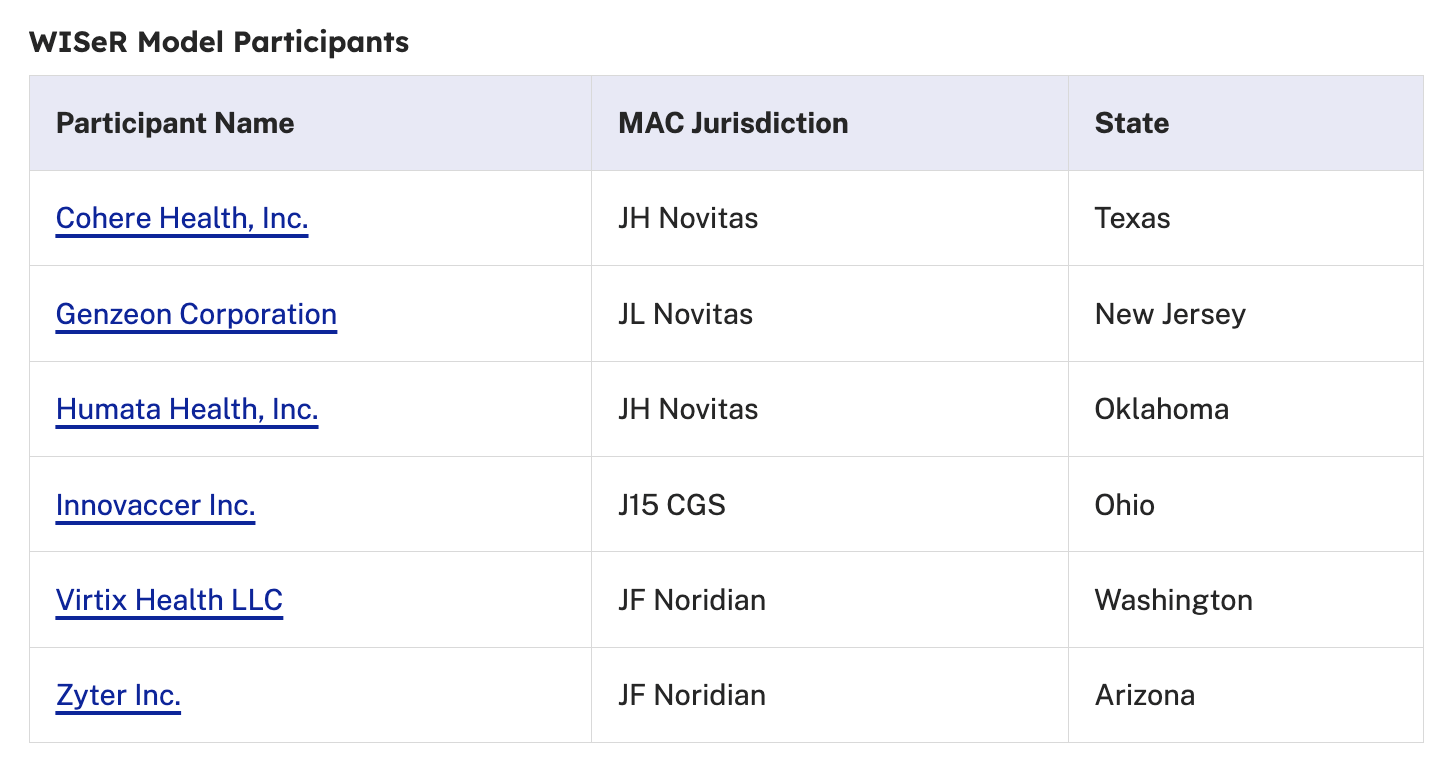
Six states—New Jersey, Ohio, Oklahoma, Texas, Arizona, and Washington—were selected to test the WISeR Model from January 1, 2026, to December 31, 2031. CMS has selected the AI vendors with experience in the AI/prior auth space who will use their technology to review claims (see below):
These companies will review prior authorizations for a laundry list of new services “prone” to unnecessary use, including services like:
skin and tissue substitutes;
implantation of electrical nerve stimulators; and
knee arthroscopy for knee osteoarthritis.
If the AI models recommend denying a prior authorization, a licensed clinician will review the AI's decision using standardized, transparent, and evidence-based procedures.
The WISeR model excludes inpatient-only services, emergency services, and services that would pose a substantial risk to patients if delayed.
Below are the model's performance measures:
Process Quality
Number of denials and favorable appeal decisions
Volume of requests processed
Provider/Supplier and Beneficiary Experience
Timeliness of response
Clarity of explanation of request determinations
Clinical quality outcomes
Use of alternative services
Evidence of ongoing urgent need to address the clinical issue
And now, the million-dollar question: how will these contracted AI companies be compensated? CMS will pay these companies a percentage of the savings from denied prior authorizations, adjusted based on the above performance measures. (Read that again—reimbursement is tied to denials).
Dashevsky’s Dissection
I understand that in a privatized, for-profit insurance system—including Medicare Advantage—prior authorization is a necessary tool to control costs and utilization. But Traditional Medicare isn't privatized (yet), and the WISeR model feels like an attempt to align Traditional Medicare's fairly robust prior authorization process with Medicare Advantage's deeply flawed one. We're importing the worst part of MA into Traditional Medicare.
So how will this impact stakeholders?
Patients
Traditional Medicare beneficiaries will face new barriers to accessing care they often need—steroid injections for joint pain, nerve stimulators, and other treatments. While none of the services listed under WISeR are medically "urgent" or "emergent," they may feel urgent to the patient experiencing pain or disability. And that matters.
A week-long delay while an AI reviews a claim, then a clinician, then an appeal, then back-and-forth—that's not patient-centered care. Especially when this barrier didn't exist before.
Physicians
Physicians who were largely unburdened by prior authorization headaches for Traditional Medicare patients will now navigate new AI-driven reviews. Orthopedic surgeons, spine surgeons, ENTs, and primary care physicians will be most affected based on the WISeR service list. They'll likely be using their own AI prior auth tools to fight with CMS's prior auth tools.
While the initial list of services isn't overwhelming—and some services are indeed high-cost, low-evidence—this could be the foot in the door for expanding prior authorization to many more services down the line. What starts as a targeted pilot could evolve into Traditional Medicare functioning like an MA plan when it comes to prior authorization.
CMS claims this will reduce administrative burden. But they’re adding burden where there was almost none. Traditional Medicare was the least burdensome payer when it came to prior authorization.
CMS and Perverse Incentives
We're letting for-profit AI contractors determine whether Traditional Medicare beneficiaries can access needed care—and compensating them with a percentage of denied claims. The incentive structure couldn’t be clearer: deny more, earn more.
We should demand transparency into these models. CMS will likely see savings through denials, but I'll be watching the clinical quality outcomes closely. What happens to patients whose care continues to be denied?
What's the Alternative?
Leave Traditional Medicare's prior authorization process alone. It works. It's accurate. It prevents waste without creating the delays and denials that plague Medicare Advantage.
Or we eliminate prior authorization entirely. But that would lead to higher premiums and lower physician reimbursement. Neither option is palatable, but importing MA's worst feature into Traditional Medicare isn't the answer either.
In summary, CMS is bringing AI-driven prior authorization to Traditional Medicare through the WISeR Model, but Traditional Medicare's prior authorization already works well with near-perfect accuracy and minimal burden. The WISeR Model adds barriers where few existed, compensates AI contractors based on denials, and imports Medicare Advantage's most criticized feature into a system that didn't need fixing. Patients will face delays, physicians will gain administrative burden, and the perverse incentive structure raises serious questions about whether this "solution" creates more problems than it solves.
P.S. I talk about all the ways AI can impact healthcare utilization in my latest course, AI and Healthcare Utilization (included with Huddle+).

FROM HUDDLE+
ACA Enhanced Subsidies Expire Dec 31: What Physicians Need to Know
Four million people may lose health insurance. Not because of a pandemic or Medicaid unwinding. Because Congress can't agree to extend the enhanced ACA subsidies that expire on December 31st, and open enrollment is already underway.
This matters to us physicians. We're about to see patients delay care, skip medications, and show up sicker because their premiums just doubled.
But the real problem isn't just about extending or not extending subsidies. Since 2014, premiums have roughly doubled, bronze plan deductibles hit $7,500, and the seven largest insurers made over $500 billion in profit—money that could have funded enhanced subsidies for the next decade.
We're stuck arguing about who should pay for broken healthcare instead of how to fix it...
👉 Full breakdown in my latest Huddle+ article here.
FROM HUDDLE UNIVERSITY
AI & Healthcare Utilization — Now Live
If you’ve been trying to separate AI hype from reality, this course is built for you.
AI & Healthcare Utilization walks through real‑world use cases across hospitals, physician groups, and payers—how AI is actually being used to reduce waste, improve flow, and support better care, with concrete ROI numbers and frameworks you can apply in your own setting.
I dig into where AI meaningfully changes utilization (and where it doesn’t), which vendors are solving real problems vs adding noise, and what it takes to go from pilot to system‑wide adoption without burning out your clinicians or blowing up workflows.
👉 Course is live—enroll in “AI & Healthcare Utilization” here.
2026 PREDICTIONS
What are your healthcare predictions for 2026?
Have any hot takes for 2026? I’m compiling my 2026 healthcare predictions report and I want to feature predictions from the community!







