INEFFICIENCY INSIGHTS
Why Getting Paid in Healthcare Is So Inefficient
Getting paid as a physician is hard. But it shouldn’t be.
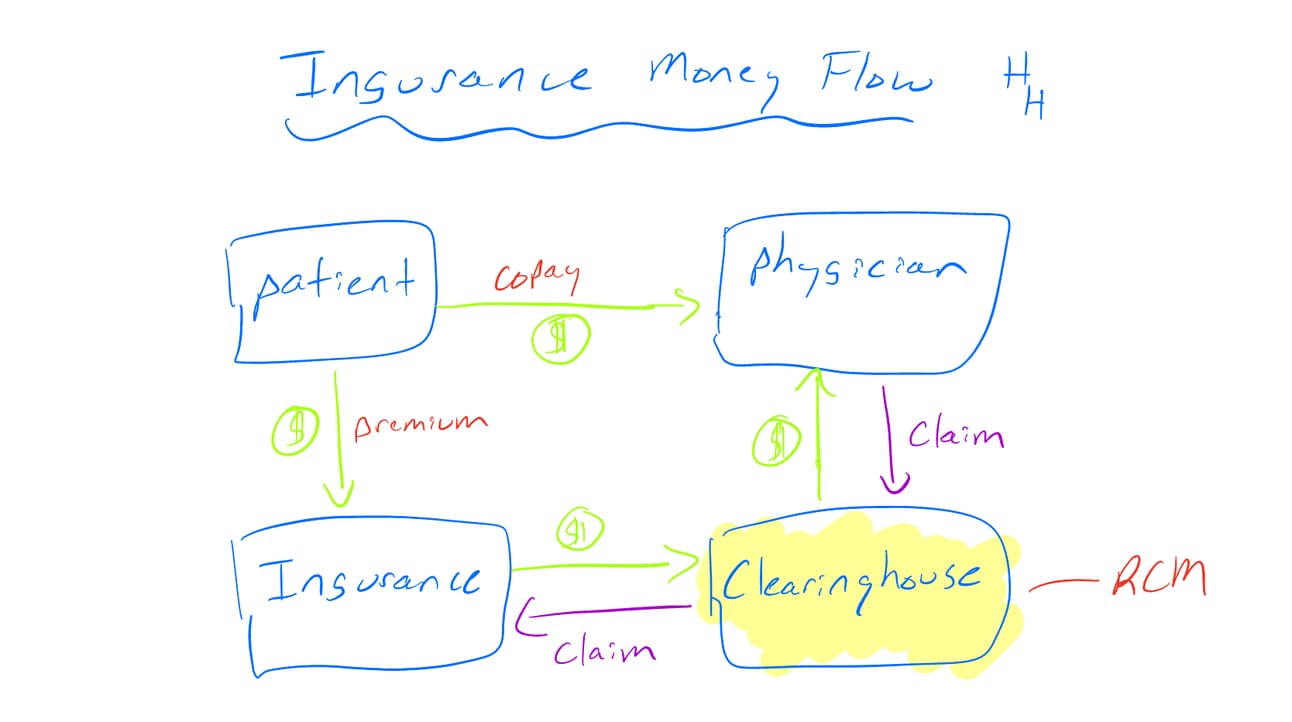
You can literally save someone’s life in the hospital, and it’ll still take 30 to 70 days to see payment—if it comes at all. There’s no direct exchange between doctor and patient like you’d expect when buying a pair of sneakers. Instead, getting reimbursed in medicine is a drawn-out, convoluted process full of middlemen and delays.
If you want a deeper dive, check out my class on Revenue Cycle Management. But here’s the short version:
It costs money to get paid. Before a claim even reaches an insurer, billing and clinical documentation improvement (CDI) teams comb through your notes to ensure maximum reimbursement. That staffing isn’t cheap. Once the bill is finalized, it’s sent to a clearinghouse (like Change Healthcare), which routes it to the right insurer and determines what they’ll pay—and what the patient owes. These intermediaries take a cut. It’s small per claim, but across billions of claims, it adds up fast.
It takes time to get paid. From the moment you submit a claim, it enters a waiting game. Prior auth holds it up. Insurers review it. Maybe it gets rejected for a minor coding issue or a mismatched modifier. You appeal, resubmit, and wait again. All the while, you’re delivering more care, generating more claims, and repeating the cycle.
You don’t always get paid. Some claims fall through the cracks. Others are denied with little explanation. Even when approved, payments don’t always reflect the time, complexity, or value of the care provided.
The administrative role of “financial transactions” make up nearly a quarter of all administrative spending.
Insights
Root Cause Analysis: 5 Whys
The 5 Whys process in root cause analysis involves repeatedly asking "Why?" five times to drill down into the root cause of a problem by exploring the cause-and-effect relationships underlying the issue.
The problem: Getting reimbursed in healthcare is inefficient, costly, and time-consuming.
Why?: The process involves multiple steps, stakeholders, and intermediaries (e.g., coders, billers, clearinghouses, insurers) which all require time and resources.
Why?: Reimbursement is based on complex coding systems (CPT, ICD, DRGs) and payer-specific rules that must be navigated to ensure payment and avoid denials.
Why?: The U.S. healthcare system lacks standardized payment models and instead relies on a fragmented mix of public and private payers, each with their own rules and incentives.
Why?: Historical decisions to tie health insurance to employment and avoid government-run universal healthcare, leading to a patchwork of insurers and administrative layers.
Why (root cause)?: Political, economic, and cultural resistance to centralized healthcare reform, which favored market-based approaches and employer-sponsored coverage over government-administered systems.
Impact Analysis
Impact analysis is the assessment of the potential consequences and effects that changes in one part of a system may have on other parts of the system or the whole.
Patient: The convoluted reimbursement process often translates into surprise bills, delayed care, and confusion over what’s covered and what isn’t. When claims are denied or payments are delayed, it can force providers to shift costs to patients or make tough choices about what services to offer.
Clinician or Provider: The burden of navigating reimbursement takes a serious toll. Time that could be spent with patients is instead diverted toward documentation, coding, and follow-ups on denied claims. It contributes to burnout, especially among smaller practices that lack large billing teams. In some cases, it discourages physicians from accepting certain insurance plans altogether, limiting patient access.
System: These inefficiencies drive up administrative costs, reduce productivity, and divert resources away from actual care delivery. Hospitals and practices must hire armies of billing staff, invest in software to manage claims, and still accept that a percentage of revenue will be lost chasing payments. Over time, this erodes trust, strains provider-payer relationships, and fuels the broader unsustainability of the U.S. healthcare system.
Solution: Direct Pulmonary Care Example
One way to escape the inefficiencies of traditional reimbursement is to sidestep the billing system altogether. That’s where Direct Care models come in—physician-led practices that cut out insurance and operate on a simple, transparent subscription model.
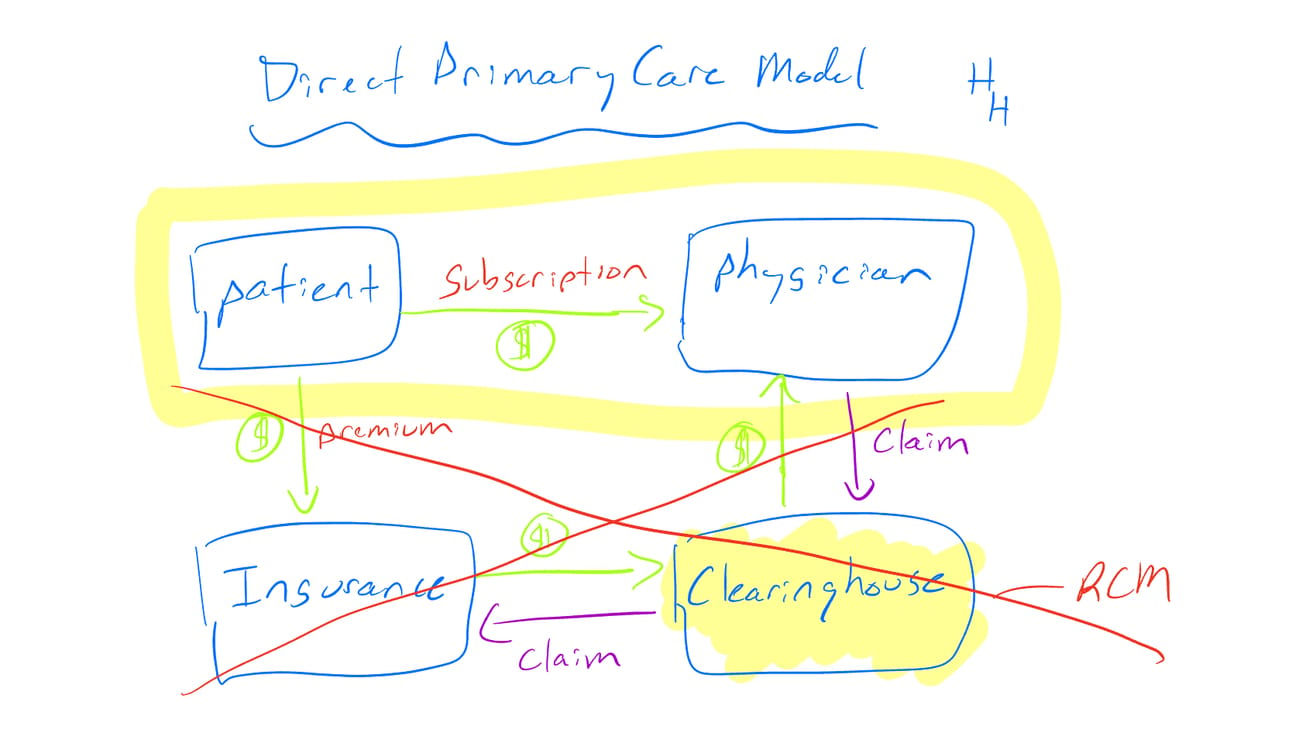
So, what would this look like for me, a future pulmonologist?
Imagine a Direct Pulmonary Care clinic where patients with chronic respiratory diseases—like COPD, asthma, pulmonary fibrosis—pay a monthly fee (say, $100–$200) for ongoing access to a pulmonologist.
Same-week in-person or virtual visits
Remote monitoring of oxygen levels or pulmonary function
Care coordination with sleep labs or home oxygen suppliers
Streamlined prescription renewals
Education on inhaler technique or pulmonary rehab
No CPT codes. No prior auths. No waiting 45 days for an insurance company to decide if I deserve to get paid. Just care—delivered directly to the patient, and supported by a sustainable financial model.
For me, that’s appealing. I’d get to work with a smaller panel of patients, spend more time with each one, and build meaningful relationships. I wouldn’t be glued to the EHR, coding every nuance of a visit just to justify a billing level.
For patients, they get transparency and access. No surprise bills. No wondering what’s covered. Just a clear monthly price for comprehensive pulmonary care. For many patients with stable but complex conditions, that kind of continuous, proactive care could mean fewer hospitalizations and better outcomes.
That said, direct care isn’t a cure-all. I’m not naive.
Some patients will still need insurance—for high-cost imaging, PFTs, biologics, or hospitalization. A Direct Pulmonary Care model wouldn’t replace insurance, but it could coexist with it. Think of it as a foundation for better outpatient management, layered with insurance for when things escalate.
There’s also the issue of equity. Not everyone can afford a monthly subscription. And if this model only ends up serving the wealthier or healthier subset of patients, it risks deepening existing disparities. That’s something I’d need to be intentional about—from pricing to partnerships to potential subsidies.
Still, the core idea is compelling: stop coding care and start delivering it. A Direct Pulmonary Care model won’t replace traditional reimbursement—but it could serve as a compelling alternative for physicians who are tired of dealing with the system and patients who are tired of waiting in it.

🔒 PREMIUM CONTENT THIS WEEK
What you’re missing
While you’re reading this, Huddle+ members are diving deeper into the topics that matter most.
Here’s what they saw this week:
The Group Bargain: How GPOs Shape the Hospital Supply Chain: Group Purchasing Organizations (GPOs) are supposed to save hospitals money. But what if they’re doing the opposite? I dive into how these middlemen operate, their controversial incentives, and why some say they’re driving up costs instead of cutting them.
Mid-Year Check-In: 2025 Healthcare Trends and Predictions Update: We’re halfway through the year—how are our healthcare trend predictions holding up? From AI and GLP-1s to policy shifts and payer moves, I break down what’s actually happening across the industry and what to keep an eye on for the rest of 2025.
How Healthcare Really Works: The system is more than just medicine. My new HuddleU course explores the hidden forces shaping healthcare: hospital finances, insurance games, drug pricing, and more. If you’re serious about understanding the business behind the practice—and want to grow your impact—upgrade here.